Learn more about PRONTO at the upcoming FIGO Conference
PRONTO International is proud to be showcasing our worldwide impact and approach to improving outcomes during childbirth at the FIGO 2015 Conference, October 4-9th in Vancouver, Canada. Join PRONTO at one of our sessions or come visit us at our booth in the exhibition hall to learn more.
PRONTO’s Approach
PRONTO International aims to optimize care during birth. We develop and implement innovative training strategies that act as a catalyst for health care providers to make individual, team, and systems changes.
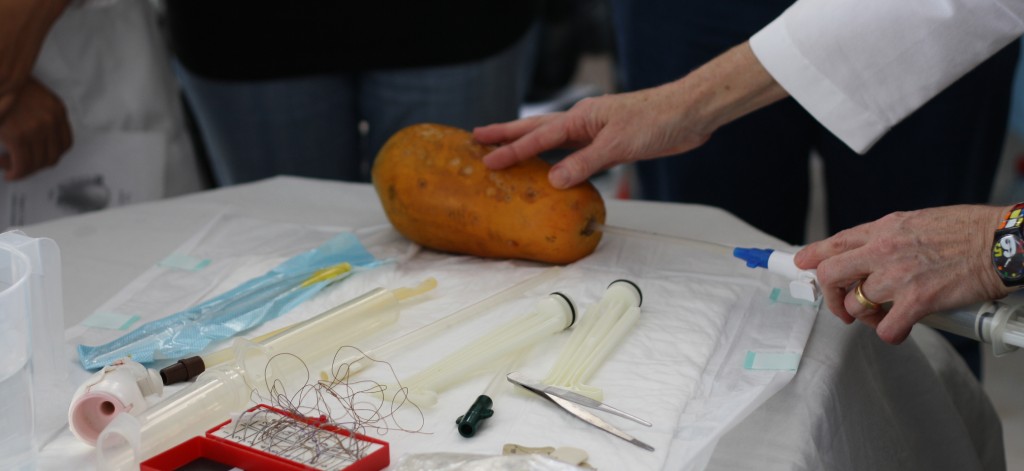
Well-trained health care providers require opportunities to practice skills in high-stress environments to ensure appropriate responses during an emergency. PRONTO’s approach to delivering simulation and team training for obstetric and neonatal emergency response in resource-limited settings moves one step closer to ensuring optimal and timely care for mothers and infants during life-threatening emergencies.
Our highly realistic simulations ask care teams to respond to, and manage emergency scenarios, and then engage in guided self-analyses of their performance through video assisted debriefing. PRONTO International has shown that the same concepts and techniques that have proven to be effective in transforming delivery of efficient and safe care for patients in high-resource settings can, and must, be applied to improve outcomes in low-resource settings. To make the training affordable and accessible, PRONTO uses low-cost portable materials.
PRONTO Panel Presentation
Tuesday, October 6:
08:00 -09:30 – West Building, Ballroom C
Using in-situ, highly realistic simulation as a scaffolding for quality improvement. Learn how simulation and team training drives quality improvement initiatives in Kenya, India, and the USA in resource-limited settings.
Abstract:
This session presents three innovative approaches to using emergency obstetric simulation and team training in resource-limited settings. We discuss the benefits, practical implications, and results of brining simulation to the actual site where the emergency occurs.
Over the last five years, PRONTO International has partnered with local organizations in seven countries to implement highly-realistic simulation and team training, improving the quality of emergency obstetric and neonatal care where it is needed most. With PRONTO, provider teams practice their emergency management skills in-situ. The resulting programs have taken on different forms catering to the local needs and limitations. Presenters will be from partner organizations who have successfully integrated simulation and team training into their programs, addressing their unique sets of priorities and obstacles. Presenters will discuss the process of simulation integration, impact on quality improvement initiatives, and lessons learned from introducing this approach.
Chairperson:
Dilys Walker, MD
Dilys Walker is Obstetrician Gynecologist, Professor, Department of Obstetrics, Gynecology & Reproductive Sciences, Bixby Center for Global Reproductive at the University of California San Francisco and founding member of PRONTO International. Prior to joining UCSF, she worked at the University of Washington and was Associate Director for the Global Center for Adolescent and Womens’ Health. She also spent 11 years at the National Institute of Public Health in Mexico, where Dilys and and her team developed this novel approach to emergency training in response to the local need to find a way to get provider teams to do what they need to do, when they need to do it, in response to an emergency to save a life. Dilys has led PRONTO’s growth from Mexico to Guatemala, Kenya, and India.
Panel Speakers:
The Western Kenya Experience: Implementing the standard PRONTO curriculum in public health clinics
Onesmus W. Gachuno, MD –University of Nairobi, Kenya
Onesmus W. Gachuno, MD, is an obstetrician/gynecologist and Senior Lecturer in the Department of OB/GYN at the University of Nairobi and consultant at Kenyatta National Hospital. He is the Kenyan Principlel Investigator for PRONTO, as well as a co-investigator of the PRONTO research project, Linda Afya ya mama na motto in Western Kenya. He is also the PI of a PEER funded impact research study of PRONTO on neonatal mortality rates within 24 hours of birth.
The PRONTO Experience: Implementing emergency obstetric simulation and team training Worldwide
Minnie W. Kibore, MBChB, MMed –University of Nairobi, Kenya, University of Washington USA
Dr. Minnie W. Kibore, MBChB, MMed (Pediatrics and Child Health) Medical Education Partnership Initiative (MEPI) program in Kenya, a collaborative partnership between the University of Washington and the University of Nairobi that aims to develop a multidisciplinary program focused capacity building and strengthening of implementation science research in Maternal Newborn and Child Health (MNCH) in Kenya. Dr. Kibore also serves as the project director of the Partnerships for Enhanced Engagement in Research (PEER) funded study that aims to study the impact of PRONTO’s emergency obstetric and newborn in-situ simulation training on maternal health n Kisii County in Kenya. Dr. Kibore is also a member of the Technical Advisory Committee overseeing the implementation of the Community Based Maternal Newborn Health project in Kakamega County, Kenya.
The Bihar, India Experience: Integrating simulation and team training into a large-scale midwife mentoring program
Dr. Sunil Kaul – CARE India, Bihar, India
Dr Sunil Kaul is an alumnus of the Armed Forces Medical College, India and completed his Masters in Public Health at the London School of Hygiene and Tropical Medicine, London. He was in the Army for ten years, where he commanded military medical units and was also involved with organising field military units in counter-insurgency operations. For over 20 years thereafter, he has worked in the rural areas of Rajasthan and Assam as a health and development professional. Sunil has been the founding trustee of the Indian NGO “the ant”, and has served in honorary capacity as the State Advisor to the Supreme Court’s Commissioners on the Right to Food and as a State Representative for the Right to Elementary Education of the National Commission for Protection of Child Rights. He partners with PRONTO International in his role at CARE India, Bihar, as a Deputy Director of Capacity Building, where he leads the team of health professionals that are involved with the BEmONC (mobile) nurses mentoring programme, and in initiating and coordinating the CEmONC Mentoring programme.
The Airlift NW Experience: Bringing emergency obstetric simulation and team training to the heliport
Lisa Ann Davidson, RN, MN, CCRN, CPNP, EMT-B– Airlift Northwest, Seattle, Washington
Lisa Ann Davidson is a Pediatric Clinical Educator and critical care Flight Nurse with Airlift Northwest with significant pediatric ICU and neonatal ICU experience. She is also a lecturer for the University of Washington, Tacoma, and is currently pursuing her Pediatric Nurse Practitioner and Doctor of Nursing Practice degrees at the University of Washington, Seattle. Lisa has overseen and manages the integration of PRONTO in-situ simulation training into AirLift Northwest’s obstetric training program, where she simulates obstetric emergencies during transport.
PRONTO Scientific Sessions
Monday, October 5:
08:00-09:30 – Room 117
Low-tech, simulation-based in service training for primary level maternity providers: Impact of the PRONTO trainings on provider knowledge and system change process indicators in Kenya (Session Name: FCS10)
Authors: Julia C Dettinger, Stephen Kamau, Kimberly Calkins, Onesmus Gachuno, Dilys Walker
Background: Appropriate and efficient responses to obstetric and neonatal emergencies are essential for improving maternal and perinatal health outcomes. Through the Linda Afya ya Mama na Mtoto project, PRONTO implemented in service trainings in emergency obstetric and neonatal care for providers at 26 primary level health facilities in Kakamega County, Kenya.
Methods: From 2013 to 2014, 177 healthcare providers participated in six PRONTO trainings in Kakamega, Kenya consisting of Modules I and II trainings, 2-3 months apart. Knowledge of obstetric hemorrhage, neonatal resuscitation, shoulder dystocia, pre-eclampsia, and teamwork concepts were assessed in addition to a teamwork self-assessment. During the Module I training, participants were asked to develop strategic goals to improve care for mothers and infants in their facilities, informed in part by their PRONTO simulation training. Completion of these goals was assessed at the Module II training, and again during follow up site visits three to eight months later.
Results: Preliminary analyses of the pre/post test scores at Module I show a 24 percentage point increase in knowledge of obstetric hemorrhage (p: <0.0001), 20.1 percentage point increase in knowledge of neonatal resuscitation (p: <0.0001), and a 23 percentage point increase in knowledge of teamwork concepts (p: <0.0001). These changes were sustained when comparing scores post Module I with post Module II (p: 0.83, 0.71, 0.62, respectively). At Module II, providers achieved 86% of the 155 strategic goals set during Module I. By the site visits, providers had developed an additional 33 goals, and accomplished 99.4% of 188 strategic goals.
Conclusions: These results suggest that PRONTO trainings are well received in Kakamega County, resulting in improved provider knowledge and a high rate of strategic goal achievement. Continued investment in trainings and provider empowerment to decide and implement changes within their facilities are required for continued improvement in maternal and perinatal health outcomes.
Monday, October 5:
08:00-09:30 – Room 116
Impact of PRONTO simulation-based obstetric and newborn care training on non-emergency delivery practices in Guatemala (Session Name: FCS07)
Authors: Anna Walton, Edgar Kestler, Julia Dettinger, Sarah Zelek, Francesca Holme, Dilys Walker
Objective: To assess the impact of PRONTO, a low-technology, simulation-based training program for obstetric and perinatal emergency management, on primary-level clinics’ non-emergency delivery practices.
Methods: Fifteen intervention clinics participated in PRONTO as part of a matched-pair cluster randomized trial in Guatemala. We conducted a cross sectional birth observation study in a convenience sample of nine clinic pairs (n=18). Study outcomes included implementation of practices previously shown to decrease maternal/neonatal mortality and improve patient care. One and two-tailed t-tests were used to compare proportional differences of practice utilization between intervention and control facilities.
Results: We observed 25 and 17 births in intervention and control clinics, respectively. Intervention teams appropriately performed active management of the third stage of labor more often than controls (83% v 50%, P=0.01) and implemented more practices proven to decrease neonatal mortality (P<0.001). They more often ensured patient privacy (92% v 65%, P=0.01) and kept patients informed (100% v. 55%, P=0.001). Differences were also noted in many teamwork-related outcomes; in particular, skill-based teamwork tools were observed more often in intervention sites (P=0.009-0.03).
Conclusions: PRONTO appears to benefit non-emergency delivery care by increasing utilization of evidence-based practices, patient-centered care, and teamwork. Further research is needed to better assess impact.
Improving Clinical Obstetric Teamwork: A Tool for Practice- Based Feedback in Low Income Countries (Session Name: FCS07.8)
Authors: John Cranmer, Jean Baumgarder, Susanna Cohen, Julia Dettinger, Edgar Kestler, Francesca Holme, Dilys Walker
Objective: Cohesive teamwork could maximize available resources and decrease obstetric-related morbidity and mortality during facility births in Low and Middle Income Countries (LMICs). However, there are no known teamwork measurement tools for these contexts. An intuitive teamwork tool for real-time feedback could foster measurement and quality improvement. As part of a larger study of PRONTO’s obstetric outcomes, this nested observational study aims to create a robust, abbreviated teamwork tool that can 1) rapidly and accurately measure clinical teamwork 2) be implemented with limited training, 3) provide real-time feedback during obstetric trainings or clinical mentorship and 4) track a facility’s skills longitudinally.
Methods: 9 simulated obstetric emergencies were managed by primary care clinicians at 7 sites from a cluster-randomized trial in Guatemala. This nested observational study analyzed 53 achieved videos of the simulation; they were coded for 57 teamwork behaviors using the Performance Assessment for Communication and Teamwork-Video tool (PACT-V) that quantifies TeamSTEPPS behaviors. Blinded bilingual coders randomly scored 77 videos. Standard exploratory, Principal Factor Analysis (PFA) with varimax orthogonal rotation and post-model decision criterion were used to extract factors and surrogate variables for a short-form of the PACT-V.
Results: Domain-specific Kaiser-Meyer-Olkin criterion (KMO) for each teamwork domain ranged from 52.04-78.59%. 10 factors and 21 surrogate variables were extracted from the 57-item PACT-V using PFA. These variables contributed to a short-form of this tool—the MOM (Measurement of Obstetric team-Managemen)t. Cohesion of the MOM’s domain-specific scales exceeded the original PACT-V tool with Alphas (α) ranging from 76.58-96.06%. The MOM’s behavioral anchors were adapted from Dreyfus’ non-judgmental scales for complex skill measurement and MOM modified the typography and structure of the PACT-V to promote intuitive use and to match “Balanced Score Card” measurements used in Kenya and other LMICs.
Conclusions: The MOM’s quantitative, simplified five-point scales and intuitive typography could promote rapid teamwork measurement at primary obstetric facilities in LMICs. The non-judgmental behavioral anchors could promote team self-reflection or non-threatening facilitator feedback during training or facility-based quality improvement coaching. The tool’s flexibility permits episodic domain-specific feedback or longitudinal coaching. Using the MOM to disseminate teamwork measurement throughout health systems could enculturate continuous improvements in obstetric quality and promote maternal-neonatal survival.
Beyond Signal Functions in Global Emergency Obstetrics: Using a Cascade Model to Improve Clinical Quality and Guide National Strategy (Session Name: FCS08)
Authors: John Cranmer, Julia Dettinger, Kimberly Calkins, Minnie Kibore, Dilys Walker
Objective: Clinical Emergency Obstetric Care (EmOC) capacity is traditionally assessed using the “Signal Functions” framework. We compared EmOC capacity using signal functions and a novel “Clinical Cascade” using two functions—retained products of conception (RPOC) and anticonvulsants. The cascade is a hierarchal model where emergency functions at the top of the hierarchy, (i.e., MgSO4 for pre-eclampsia), cannot be performed without requisite resources. The cascade has five stages: 1) identification (e.g., sphygmomanometer-stethoscope for pre-eclampsia), 2) consumables (e.g., IV supplies), 3) durables (e.g., IV poles) and 4) medications (e.g., MgSO4). Stage 5—monitoring & modifying interventions, is crucial for quality but considered separately.
Methods: This cross-sectional facility analysis, nested within a non-equivalent group design pre-post implementation trial in Kakamega County, Kenya, summarized 758 facility-specific variables from 42 basic EMoC clinics. 276 of these variables relate to five elements of EMoC care (Facilities, Staff, Equipment, Supplies, Drugs). We described these resources using a standard adaptation of signal functions and tracer drugs. Subsequently, we compared these findings to a facility’s practical EmOC capacity using a novel cascade model adapted from HIV and the “Hierarchy of Needs.” The proportion of facilities with EmOC resources at each stage of the cascade is compared to the signal function analysis.
Results: For the management of pre-eclampsia, 71.4% of facilities had the first-line signal function tracer drug available. The cascade suggests 14.3% of facilities have all requisite resources for pre-eclampsia management, while 4.3% of facilities could monitor and modify therapy. 38.1% of facilities have stage 1 resources to identify the disorder. 31.0% have the stage 2 consumables for management; 23.8% have stage 4 durable equipment. 14.3% of facilities can administer stage 4’s first-line medication even though 71.4% of facilities stock it. A similar trend of step-wise decreases in resource availability is present for RPOC: 1 (100% available)à2 (90.5%)à3(47.6%)à4 (0%)à5 (0%).
Conclusions: Comparing the performance of existing signal functions and the novel cascade identifies five themes. First, the cascade identifies substantive drop-offs in EmOC resources by stage. Second, it quantitatively summarizes the precise points where resource attrition occurs. Third, using signal functions alone to assess EmOC may significantly overestimate capacity. Fourth, applying the cascade to all signal functions and diverse contexts could further refine the model. Finally, this cascade could enable EmOC facilities, clinicians, and health system planners to more precisely identify, measure, and improve a facility’s capacity to manage obstetric emergencies and promote global maternal survival.
PRONTO International Booth
Booth 641 in the Exhibition Hall